The intragastric balloon is one of the latest advancements in the ongoing fight against obesity. It is a procedure in which a balloon is inserted in the body to curb the patient’s appetite. Approved by the FDA in August 2015, it’s causing a lot of excitement for people who are looking to lose about 20-30 lbs., to regain their physical health. We spoke to renowned surgeon Dr. Spencer Holover, who’s clinic is the only one in the country approved to conduct the gastric balloon surgery with both balloons that are available on the market. In an exclusive interview with Raha Lewis at Connectwithlife, he spells out the pro’s and con’s of this new procedure and how it can help you get the body you’ve always wanted.
 CONNECT WITH LIFE: What exactly is the Gastric Balloon?
CONNECT WITH LIFE: What exactly is the Gastric Balloon?
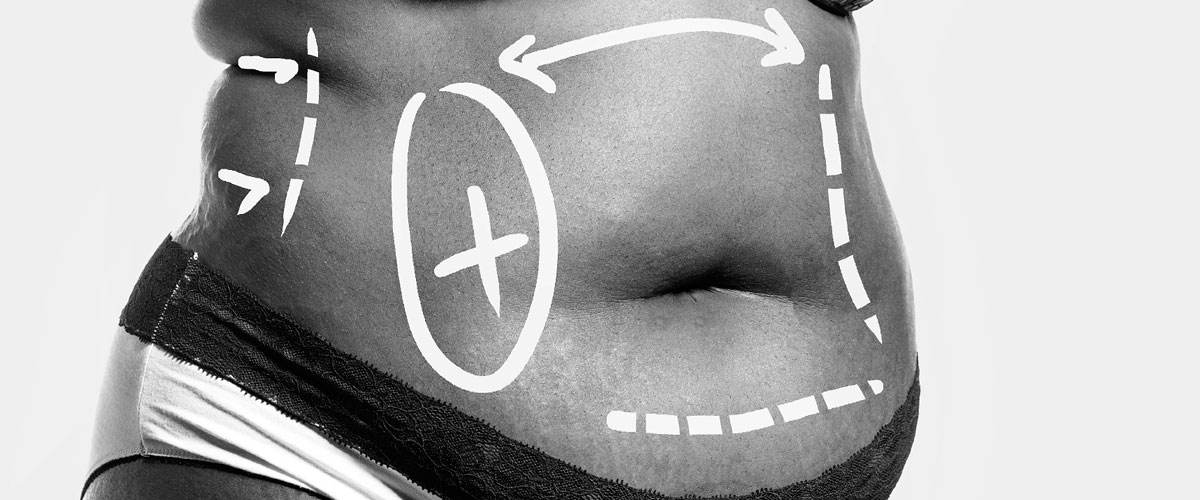
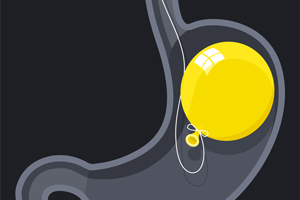
SH: It’s a weight loss procedure. It’s not considered bariatric surgery, more of a weight loss procedure. It is a device that is inserted using an endoscope – a camera that’s passed down through the mouth into the esophagus and into the stomach. The balloon is inserted using this device into the stomach, so there are no incisions and very little recuperation. It is considered a minimally invasive procedure. So much so, that I would say it’s more of a cosmetic procedure.
CONNECT WITH LIFE: How so?
SH: Traditionally bariatric surgery is considered to be a medical procedure, because you are doing it to either cure or prevent conditions associated with being overweight like diabetes, high blood pressure, sleep apnea and polycystic ovary syndrome. This is a device that is what we call ‘off label,’ which means it has never been studied to be used on patients with those medical problems.

CONNECT WITH LIFE: So who is this procedure for?
SH: This procedure is for patients who are between 10 to 60 pounds overweight with really none of the medical problems I mentioned above. It is meant strictly as a weight loss procedure, it’s not a medical procedure.
CONNECT WITH LIFE: Who is the ideal candidate besides the person who is between 10-60 pounds overweight?
SH: The way we determine who qualifies for it is through body mass index. A normal BMI is between 20-25. The BMI for ideal candidates for the surgery is usually between 30-40 but with none of the medical problems we were talking about above.
CONNECT WITH LIFE:What about being a non-smoker? Should you be fit? Should you be mentally sound?
SH: Patients who are smokers can get this device, patients who previously had bariatric surgery, depending on what kind, may not qualify for this device. But the vast majority of patients that have a BMI between 30 and 40 are definitely qualifiers as long as they don’t have any of the medical problems we talked about before. Say you have someone with a BMI of 35 or greater and they have any of those medical problems than they would probably be more suited to have traditional bariatric surgery than the balloon.
CONNECT WITH LIFE: Do you need a general or a local anesthetic?
SH: That depends on whom you ask because it is such a new procedure. Some people put the balloon in under sedation, kind of what we call like a twilight state. In my practice we use sedation we don’t use local anesthesia. Some people are doing it under general where you put a tube down and the patients are completely under general anesthesia. It depends how comfortable the anesthesiologist is. Our anesthesiologist happens to be in my experience, one of the best I have ever worked with.
CONNECT WITH LIFE: How long does the procedure take?
SH: Usually it takes anywhere between 10-20 minutes
CONNECT WITH LIFE: What is the recovery time?
 SH: Recovery time is immediate. They wake up and feel completely normal within 15 minutes of waking up. The issue with the procedure though, is that almost every patient from a period of 6-7 days will be miserable.
SH: Recovery time is immediate. They wake up and feel completely normal within 15 minutes of waking up. The issue with the procedure though, is that almost every patient from a period of 6-7 days will be miserable.
CONNECT WITH LIFE: What do you mean? What are the symptoms during those few days?
SH: Nausea, vomiting and cramping are classic symptoms. It’s the stomachs way of adjusting to the balloon being in there.
CONNECT WITH LIFE: Is there medication they can take to ease that pain?
SH: We use four different medications, we use a medication called zofran which is an anti-nausea medication it is also used on cancer patients. We also use something called a protonic which decreases the amount of acid in the stomach. We also use levsin which calms the GI track down, and we also use xanax to relax the patient after the surgery and make them a lot less anxious.
 CONNECT WITH LIFE: Will the patient be able to walk right after?
CONNECT WITH LIFE: Will the patient be able to walk right after?
SH: Yes, the patient does not start feeling the nausea, stomach spasms, or pains until about five or six hours after surgery. It could be a day after and it usually lasts three to seven days.
CONNECT WITH LIFE: Does the stomach swell at all?
SH: It is not even that the stomach swells it’s more that the stomach is accommodating the balloon and conforming to it.
CONNECT WITH LIFE: Once the balloon is in and the cramping is over, what happens to the patient? What do they eat? What do they do?
SH: The patient for the first week should be on a liquid only diet. The balloon works in a couple of ways. Because it takes up room in the stomach, you needs less food to make you feel full. The other way it works is that the balloon is there so the food has to travel around the balloon to get to the stomach taking longer to go through the stomach so people feel fuller longer. It’s a combination of both of these things.
The way we do it is by telling the patients they should be on a liquid diet for a week after the surgery and then in the second week they should be on a mushy food diet, what we call a ‘stage two’ diet. So anything you don’t have to chew, almost like baby food consistency. In the third week, they can start eating regular solid foods. We tell patients if they are tolerating any of these diets really well then they can move a little faster, but we traditionally tell them one week of liquids, one week of mushy foods, and one week of solid foods.
CONNECT WITH LIFE: When can they go back to work?
SH: They can go back when they feel up to it. If they don’t have any of the nausea or stomach problems they can go back the next day, usually we do procedures on a Thursday and by the following Thursday or Friday, patients are more than fine to go back to work.
CONNECT WITH LIFE: When you say nausea and vomiting in the first week, are they able to keep anything down, or nothing?
SH: They have to keep at least liquids down because if they don’t they will become dehydrated, and then that becomes a problem.
CONNECT WITH LIFE: What if the do get dehydrated?
SH: Fortunately we haven’t had that happen yet. They key to preventing that is warning all patients to expect to have this. As far as the patients, we only had a couple that called us and said ‘I can’t deal with this,’ and we managed to talk them off the ledge. The key to our success and not having to take any of these out, is having our staff call them everyday before hand, to reassure them, and to coach them through the first few days. So far it’s worked well and we haven’t had to take any out.
 CONNECT WITH LIFE: How long does the balloon stay in?
CONNECT WITH LIFE: How long does the balloon stay in?
SH: The key with the balloon is that it needs to come out within 6 months. It cannot stay in longer than that. That is the most important point we tell our patients, it has never been trialed for more than 6 months. It’s because after 6 months, the stomach can be a very hostile environment, between the stomach acid, the mulching and other enzymes. Theoretically with a balloon in there, the hostile environment could cause the balloon to rupture and if the balloon ruptures, it can migrate and end up in the small intestine. If that were to happen sometimes it would just pass, but other times it could cause a blockage and that would be a surgical emergency.
CONNECT WITH LIFE: Has that ever happened with the balloon being in there for less than 6 months?
SH: No, what you do is there are two different balloon designs. One made by a company called Apollo Med they have a balloon that is a single balloon it looks just like a breast implant. The company that used to produce this balloon is Allergan, one of the leading producers of Botox and breast implants. They sold the concept to a smaller company called Apollo Med so there’s a single balloon, and the other, well there are only 2 approved in this country, the other is called Reshape Balloon and it has a very different design. The single balloon is one balloon and the Reshape is a dual balloon almost like two balloons attached to a dumb bell. In order to find out if they rupture, we fill them up with methionine blue, so if the balloon ruptures the methionine blue is absorbed into the blood stream and then the patient will pee out green. So if the patient calls and says ‘Doc I am peeing green,’ then we know the balloon ruptured. We take an x-ray to see if the balloon ruptured and then right away we would go back in and pull the balloon out. It should be done within a couple days to avoid it migrating to the small intestine.
CONNECT WITH LIFE :Has that ever happened? When do you use which balloon?
SH: No. Some doctors believe that the dual balloon has better contours for the stomach and therefore doesn’t move around as much. The single balloon bounces around more, but then again some people think the dual balloon causes more ulcers or sores inside of the stomach. So they both have pros and cons.
CONNECT WITH LIFE:Which one do you use?
SH: Both, we are the only practice in the entire country that is certified to do both.
 CONNECT WITH LIFE: Let’s say the patient is overweight and is training in boxing to loose weight and they get hit would the balloon rupture?
CONNECT WITH LIFE: Let’s say the patient is overweight and is training in boxing to loose weight and they get hit would the balloon rupture?
SH: No, the balloon is unbelievably strong. The chances of the balloon rupturing from a fish bone a patient swallows are minuscule. The spine or sharp substance would have to be held tight and pressed against the balloon. When we retrieve the balloon we have to pop it and it is not easy.
CONNECT WITH LIFE: So they eat less when they have the balloon, but is it uncomfortable? Do they get acid reflux?
SH: Acid reflux is one of the main problems, that’s why we give them protonics for a full 6 months. Reflux can be a problem but they can double the protonics and the reflux almost always resolves. The key with the balloon is follow up. It’s a 12 month program. Before the procedure patients meet with the nutritionist to go over the dietary guidelines and this is critical. We put the balloon in and then they follow up with us for 12 months. They see either myself or the physician assistant or a nutritionist once a month for 12 months. We take the balloon out at the 6-month mark and then they continue to see us for the next 6 months, which is critical. They also need to see a psychologist as well.
CONNECT WITH LIFE: Why a psychologist?
SH: Just to keep patients on the path and make sure they aren’t trying to substitute other types of behaviors that made them overweight in the first place. It keeps them on track. When they follow up, they just wind up doing a lot better than patients who don’t.
 CONNECT WITH LIFE: Are there risks/complications that you haven’t mentioned?
CONNECT WITH LIFE: Are there risks/complications that you haven’t mentioned?
SH: Yes, with every procedure there is risks. Some are when you are putting in the balloon, putting it down can cause damage to the esophagus or vocal chords. statistics show these occur in less than 1%. We have never had it happen. The other risk is if we tell patients they need to be on a pure liquid diet or clear liquids before the diet, and they have food in their stomach they can throw it up and it could go into their lungs causing pneumonia or even cause a blockage and they can aspirate. We put a camera down before to see if the stomach is empty. A lot of our patients are heavy and they like to eat. Some patients you go put a camera down and there stomach is full of food. We have to pull the scope out and not do the balloon. We will be like ‘listen you can die by eating before the procedure. Your stomach has to be empty when we put this in.’ Also when we take the balloon out they can’t have anything to eat or drink so that’s where the biggest risk is when we take the balloon out and if there is food around, there’s a possibility of it going into the lungs and that can be very dangerous. You tell the patient they need to have a liquid diet a couple days before the balloon comes out and if we put the camera down and see food we don’t take it out that day.
CONNECT WITH LIFE: How much does this cost?
SH: It varies from surgeon to surgeon fortunately we have our own endoscopy so we can do it in our office making us a lot more cost effective. Some people charge up to $11k. We charge between $7,500-$9,000, that includes everything; consultations with the doctor, nutritionist, anesthesia, the balloon, following ups with patients for 12 months and taking the balloon out.
CONNECT WITH LIFE: Men and women can both do this?
SH: Yes. But we won’t do it on anyone under 18.